Healthcare Reimbursement Market Research, 2033
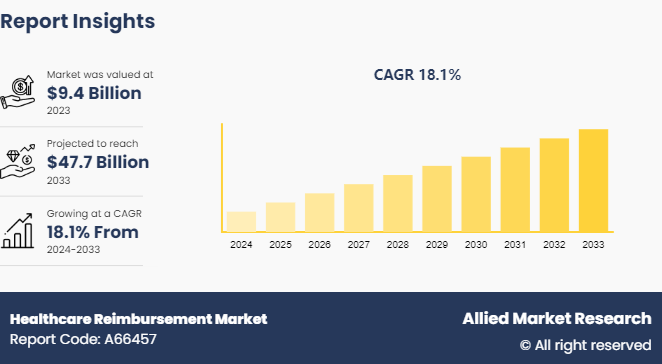
The global healthcare reimbursement market size was valued at $9.4 billion in 2023 and is projected to reach $47.7 billion by 2033, growing at a CAGR of 18.1% from 2024 to 2033.The increasing focus on value-based care and cost-efficiency in healthcare is driving the growth of the market.
Market Definition and Overview
Healthcare reimbursement is the payment that hospitals, doctors, and other healthcare providers receive for delivering medical services to patients. This compensation can come from various sources, including government programs like Medicare and Medicaid, private health insurance plans, and patients themselves. The reimbursement process involves submitting claims based on the services provided, which are then evaluated and paid according to predetermined rates and agreements. Efficient reimbursement systems are crucial for ensuring healthcare providers are compensated fairly and promptly, which helps maintain the financial viability of healthcare facilities and ensures patients have access to necessary medical care. Reimbursement methods vary, including fee-for-service, bundled payments, and value-based care models.
Key Takeaways
- The healthcare reimbursement market size study covers 20 countries. The research includes a segment analysis of each country in terms of value ($billion) for the projected period from 2024 to 2033.
- More than 1, 500 product literatures, industry releases, annual reports, and other such documents of major healthcare reimbursement industry participants along with authentic industry journals, trade associations' releases, and government websites have been reviewed for generating high-value industry insights.
- The study integrates high-quality data, professional opinions and analysis, and critical independent perspectives. The research approach intends to provide a balanced view of global markets and assist stakeholders in making informed decisions in order to achieve their most ambitious growth objectives.
Market Dynamics
Rising healthcare service and product expenses are driving demand for effective reimbursement systems. In addition, increasing prevalence of government-led healthcare programs is anticipated to further boost the healthcare reimbursement market growth. Innovations and technological advancements in healthcare services also contribute to the growth of this market. Overall, these factors collectively highlight the dynamic nature of the healthcare reimbursement market, where increased financial demands and governmental initiatives lead to progress, while technological advancements enhance efficiency and service delivery.
The healthcare reimbursement market faces significant restraints due to high administrative costs. The complexity and administrative burden of processing reimbursement claims lead to increased operational expenses. This inefficiency can strain healthcare providers and payers, reducing overall profitability and potentially hindering market growth. Simplifying administrative processes and reducing associated costs are essential to overcoming these challenges and supporting the market development.
Rapidly changing lifestyles and widespread occurrence of chronic disorders such as diabetes, heart ailments, and cancer, are driving up medical costs and increasing demand for healthcare reimbursement. Government initiatives that support healthcare insurance to cover these costs are also contributing to market growth. In the U.S., the Affordable Care Act aims to expand healthcare insurance coverage for low-income individuals, further boosting market prospects. In addition, rising healthcare costs, an increasing number of patients, and higher consulting fees for physicians, medications, and treatments are expected to boost healthcare reimbursement market share expansion in the upcoming years.
Public Policies in the Global Healthcare Reimbursement Market
Public policies play a crucial role in shaping the global healthcare reimbursement market. Here are some key points:
- Insurance Mandates: Government policies mandating healthcare insurance coverage influence reimbursement dynamics by expanding the pool of insured individuals, thereby leading to an increase in demand for reimbursement services.
- Regulatory Frameworks: Regulatory bodies establish guidelines and standards for reimbursement processes to ensure transparency, fairness, and efficiency. Compliance with these regulations is essential for healthcare providers and payers.
- Healthcare Financing Models: Public policies often dictate the structure of healthcare financing models, such as single-payer systems, private insurance, or a combination of both. These models determine how healthcare services are funded and reimbursed.
- Affordability Initiatives: Governments implement affordability initiatives to make healthcare services more accessible and affordable to all citizens. These policies may include subsidies, price controls, or reimbursement programs for low-income individuals.
- Technology Adoption Incentives: Public policies may incentivize the adoption of technology in healthcare reimbursement processes to improve efficiency, accuracy, and transparency. This could include funding for electronic health record systems or telemedicine platforms.
Market Segmentation
The market is segmented into claim, payer, service provider, and region. On the basis of claim, the market is divided into underpaid and full paid. As per payer, the market is classified into private payers and public payers. On the basis of service provider, the market is divided into physician office, hospitals, diagnostic laboratories, and others. Region wise, the market is analyzed across North America, Europe, Asia-Pacific, and LAMEA.
Regional Market Outlook
The increasing prevalence of chronic diseases and rising healthcare reimbursement costs boost the demand for reimbursement services in North America. Government initiatives, such as the Affordable Care Act in the U.S., expand healthcare insurance coverage, further boosting the regional healthcare reimbursement market share. In addition, advancements in healthcare technology and rising aging population contribute to the expansion of reimbursement solutions in the region.
- In August 2023, Codoxo, a U.S.-based AI specialist, unveiled ClaimPilot, a generative AI solution. ClaimPilot targets enhanced efficiency in healthcare cost containment and payment integrity programs, addressing workforce constraints. Initially focusing on in-patient and facility claim audits, it aims to significantly accelerate audit turnaround times and clinician audits per day. Moreover, ClaimPilot removes dollar thresholds, broadening claims analysis to encompass lower dollar ranges for increased accuracy and coverage.
Competitive Landscape
The major players operating in the healthcare reimbursement market include UnitedHealth Group, The Blue Cross Blue Shield Association, Aetna, AgileHealthInsurance, Aviva, WellCare Health Plans, Allianz, BNP Paribas, Nippon Life Insurance, CVS Health, and others.
Recent Key Strategies and Developments
- In March 2022, Icertis introduced Icertis Contract Intelligence (ICI) for Healthcare Providers, a contract lifecycle management (CLM) solution. This platform aids healthcare providers in expediting digital transformation efforts by modernizing intricate agreements, including those with payers, suppliers, and contract services.
- In August 2021, Baring Private Equity Asia (BPEA) , a prominent private alternative investment firm in Asia, finalized agreements with Hinduja Global Solutions to acquire its Healthcare Services business. This acquisition, facilitated through funds associated with BPEA, is expected to boost the expansion of the healthcare payer services industry.
Industry Trends
- In March 2022, IMAT Solutions launched a new offering for healthcare data collection, aggregation, distribution, and reporting. This innovation benefits payers, statewide entities, and Health Information Exchanges (HIEs) . Their new clustering and SaaS-based solutions, along with recent Data Aggregator Validation (DAV) recognition from NCQA, highlight their commitment toward enhancing healthcare data management and quality reporting.
- In July 2021, Greenberg Advisors, a U.S.-based strategic M&A services provider, acquired Medical Reimbursement, a U.S.-based medical billing services provider, for an undisclosed amount. This acquisition aims to enhance Greenberg Advisors' capabilities and improve their service to patients by integrating Medical Reimbursement's expertise in medical billing and reimbursement services.
Key Sources Referred
- Annual Reports
- Investor Presentations
- Press Releases
- Research Papers
- D&B Hoovers
- Healthcare Reimbursement Investment & Trade Reports
- Government Publications
- Industry Publications and News Outlets
Key Benefits For Stakeholders
- This report provides a quantitative analysis of the market segments, current trends, estimations, and dynamics of the healthcare reimbursement market analysis from 2023 to 2033 to identify the prevailing healthcare reimbursement market opportunity.
- The market research is offered along with information related to key drivers, restraints, and opportunities.
- Porter's five forces analysis highlights the potency of buyers and suppliers to enable stakeholders make profit-oriented business decisions and strengthen their supplier-buyer network.
- In-depth analysis of the healthcare reimbursement industry segmentation assists to determine the prevailing market opportunities.
- Major countries in each region are mapped according to their revenue contribution to the global healthcare reimbursement market forecast period.
- Market player positioning facilitates benchmarking and provides a clear understanding of the present position of the market players.
Apart from the points mentioned above, the report includes the analysis of the regional as well as global healthcare reimbursement market trends, key players, market segments, application areas, and market growth strategies.
Healthcare Reimbursement Market Report Highlights
| Aspects | Details |
| Market Size By 2033 | USD 47.7 Billion |
| Growth Rate | CAGR of 18.1% |
| Forecast period | 2024 - 2033 |
| Report Pages | 290 |
| By Claim |
|
| By Payer |
|
| By Service Provider |
|
| By Region |
|
| Key Market Players | CVS Health, Allianz, The Blue Cross Blue Shield Association, Nippon life insurance, BNP Paribas, AVIVA, Aetna, Agile Health, UnitedHealth Group, WellCare Health Plans |
The global healthcare reimbursement market is trending towards value-based care models, increased adoption of telemedicine, expansion of insurance coverage, and advanced healthcare technologies, enhancing patient outcomes and cost-efficiency.
The leading application of the Healthcare Reimbursement Market is in insurance claims processing, where healthcare providers and insurers manage and streamline payments for medical services, enhancing efficiency and reducing administrative costs.
North America is the largest regional market for Healthcare Reimbursement Market
The healthcare reimbursement market was valued at $9.4 billion in 2023 and is estimated to reach $47.7 billion by 2033.
The major players operating in the healthcare reimbursement market include UnitedHealth Group, The Blue Cross Blue Shield Association, Aetna, AgileHealthInsurance, Aviva, WellCare Health Plans, Allianz, BNP Paribas, Nippon Life Insurance, CVS Health, and others.
Loading Table Of Content...



