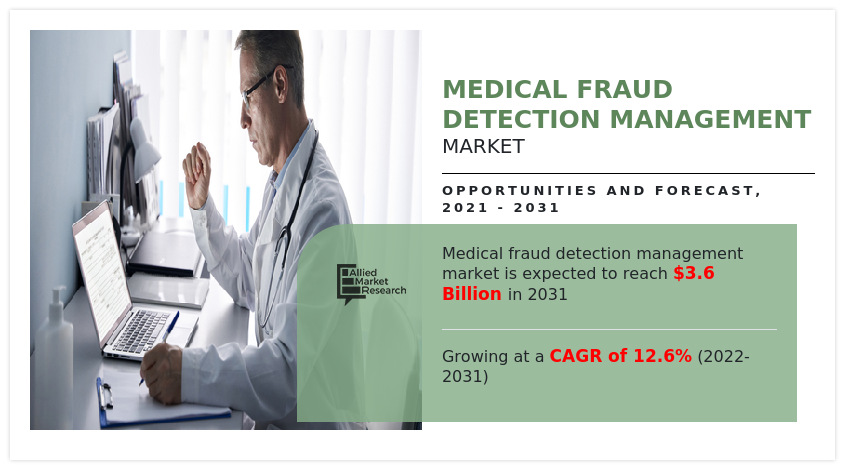
Healthcare Fraud Detection Market Research, 2031
The global healthcare fraud detection market size was valued at $1.1 billion in 2021, and is projected to reach $3.6 billion by 2031, growing at a CAGR of 12.6% from 2022 to 2031. Healthcare fraud detection involves account auditing, medical claim auditing and auditing of healthcare funds. The medical fraudulence cases, such as healthcare funds fraudulence, claims and healthcare insurance fraudulence are increased in healthcare sector. In addition, healthcare fraud detection market actually helps in preventing healthcare fraud, waste, and abuse. Healthcare fraud is completely a misrepresentation or intentional deception of facts by healthcare professionals or patients, which can be led to unauthorized payments or benefits. Some examples of healthcare frauds are including falsified data by physicians, multiple claims filed by different providers for the same patients, submitting claims for services which are not provided, misrepresenting dates in various treatments, frequency, and duration or description of services provided.
The healthcare fraud detection market size is projected to experience rapid growth, as the various new software based on data mining and artificial intelligence are being used by the healthcare industry. Furthermore, this market is anticipated to advance due to the expansion of analysis, services, insurance claim reviews and by maintaining payment integrity. Moreover, the global healthcare fraud detection market share is expanding due to increased fraud in healthcare domain, increase in pressure of abuse and fraud, and rise in patient benefiting by health insurance. Morover, as the various new software based on data mining and artificial intelligence are being used by the healthcare industry is boosting the market growth. Furthermore, this market is anticipated to advance due to the expansion of analysis, services, insurance claim reviews and by maintaining payment integrity.
Moreover, increase in use of advanced analytics, machine learning and artificial intelligence boosting the growth of the market. However, increase in data breaches in healthcare industry and lower awareness level regarding healthcare fraud analytics solutions in emerging countries is expected to restrain the healthcare fraud detection market growth. The increase in number of fraudulent activities in healthcare, rise in the number of patients seeking healthcare insurance are the major driving factors and will boost the market growth during the healthcare fraud detection market forecast.
Impact of COVID-19 on the Market
Coronavirus Severe acute respiration syndrome (SARS-CoV-2) is an infectious disease caused by the novel coronavirus (COVID-19), which originated in the Wuhan district in China in the late 2019, and since has spread to 212 countries. The virus was initially referred to as “novel coronavirus 2019” (2019-nCoV) by the WHO, However, on February 11, 2020, it was given the official name of SARS-CoV-2 by the International Committee on Taxonomy of Viruses. WHO declared COVID-19 as pandemic on March 11, 2020, and by September 1, 2020, over 28.1 million people have been infected globally with over 909,000 deaths. COVID-19 symptoms include fever, cough, and shortness of breath.
Nearly all industries have been impacted by the global public health epidemic COVID-19. As coronavirus crises sweep the globe and force healthcare organizations to devote the majority of their funds to fight COVID-19, the outbreak of COVID-19 has resulted in a significant decline in demand for the healthcare fraud detection market across several sectors, particularly the health and pharmaceutical sector. The main cause of the interruptions experienced by the healthcare payer and government agencies. As a result, the COVID-19 outbreak will slow global market growth of healthcare fraud detection, which will have a negative effect on the market's value in 2021 and beyond.
The healthcare fraud detection market is segmented into Application, End User, Type and Component.
The healthcare fraud detection market is segmented on the basis of type, component, application, end user, and region. By type, it is divided into descriptive analytics, predictive analytics and prescriptive analysis. By component, it is bifurcated into services and software. By application, the market is classified into insurance claims review and payment integrity. By end user, the market is categorized into healthcare payer (Public Payer and Private Payers), government agencies, and others. Region wise, the market is analyzed across North America, Europe, Asia-Pacific, and LAMEA.
By Type Segment Review
By type, descriptive analytics segment was the highest revenue contributor to the market. The growth of this segment is increased owing to high demand of descriptive analytics-based service across U.S and European countries.
By Type
Descriptive Analytics segment held a dominant position in 2021 and would continue to maintain the lead over the forecast period.
By Component Segment Review
By type of component, the software segment was the highest revenue contributor to the market. As majority of the medical industries use the software-based fraud detection techniques. The market growth of the segment driven by use of newly developed software based on machine learning and artificial intelligence.
By Component
Software segment is projected as one of the most lucrative segment.
By Application Segment Review
By application type, the insurance claims review was the highest revenue contributor to the market. Furthermore, most of the medical fraudulence is observed in the healthcare insurance therefore, insurance claims review generated the greater revenue and contribute to the growth of global healthcare fraud detection market. The payment integrity held the fastest growing segment.
By Application
Insurance Claims Review segment held a dominant position in 2021 and would continue to maintain the lead over the forecast period
By End User Segment Review
By end user the market is classified into healthcare payer, government agencies and others. The healthcare payer was the highest revenue contributor to the market. Furthermore, the government agencies also contributed to the global market growth.
By End User
Healthcare Payer segment is projected as one of the most lucrative segment
Region Type Segment Review
Region wise, in healthcare fraud detection industry, North America was the highest revenue contributor. As the fraudulence cases observed in the U.S and Mexico was highest in past few years. Moreover, the innovative analytical techniques and software use is increasing in the North America which is driving the market growth.
By Region
North America was holding a dominant position in 2021 and would continue to maintain the lead over the analysis period.
Major key players that operate in the global healthcare fraud detection market are CGI Group, Conduent, DXC Technology Company, EXLSERVICE Holdings Inc., Fair ISAAC Corporation, HCL Technologies, International Business Machines Corporation (IBM), LexisNexis, McKesson Corporation, Northrop Grumman, Optum, OSP Labs, SAS Institute Inc., Scioinspire CORP., UNITEDHEALTH Group, Verscend Technologies, and WIPRO Limited.
Key Benefits For Stakeholders
- This report provides a quantitative analysis of the market segments, current trends, estimations, and dynamics of the healthcare fraud detection market analysis from 2021 to 2031 to identify the prevailing Healthcare Fraud Detection Market opportunity.
- The market research is offered along with information related to key drivers, restraints, and opportunities.
- Porter's five forces analysis highlights the potency of buyers and suppliers to enable stakeholders make profit-oriented business decisions and strengthen their supplier-buyer network.
- In-depth analysis of the healthcare fraud detection market segmentation assists to determine the prevailing market opportunities.
- Major countries in each region are mapped according to their revenue contribution to the global market.
- Market player positioning facilitates benchmarking and provides a clear understanding of the present position of the market players.
- The report includes the analysis of the regional as well as global healthcare fraud detection market trends, key players, market segments, application areas, and market growth strategies.
Healthcare Fraud Detection Market Report Highlights
| Aspects | Details |
| Market Size By 2031 | USD 3.6 billion |
| Growth Rate | CAGR of 12.6% |
| Forecast period | 2021 - 2031 |
| Report Pages | 310 |
| By Component |
|
| By Application |
|
| By End User |
|
| By Type |
|
| By Region |
|
| Key Market Players | SAS Institute Inc., CGI Inc., SCIO Inspire, Corp., Fair Isaac Corporation, DXC Technology Company, LexisNexis, Optum, Wipro Limited, UnitedHealth Group, OSP Labs, Verscend Technologies, HCL Technologies, McKesson Corporation |
Analyst Review
This section provides various opinions of the top-level CXOs in healthcare fraud detection market. In accordance with several interviews conducted, the utilization of software services is likely to witness a significant growth in the market. The healthcare fraud managed by descriptive analytics, predictive analysis and prescriptive analysis. Introduction of various new software and technologies lead to the expansion of the global healthcare fraud detection market.
Increase in number of fraudulence in the medical claims and health insurances are expected to grow in the future. Also, surge in pressure of fraud and abuse of healthcare are projected to expand the market growth. For instance, the services of software and breakthrough inventions in artificial intelligence is projected to drive the global healthcare fraud detection market growth.
According to the perspectives of CXOs of leading companies in the market, developing the new innovative methods for fraud detection in healthcare industry. Rapid growth was observed in the adoption of services and software by the healthcare payer and government agencies. As per CXOs, although North America and Asia-Pacific are expected to dominate the global healthcare fraud detection market during the forecast period, emerging countries in Latin America are expected to offer significant growth opportunities in the near future.
The upcoming trends of healthcare fraud detection market are increase in number of fraudulent activities in healthcare, rise in the number of patients seeking healthcare insurance.
The leading application of healthcare fraud detection market are preventing healthcare fraud, waste, and abuse.
North America is the largest regional market for healthcare fraud detection.
Healthcare fraud detection is projected to reach $3,600.0 million by 2031.
Major key players that operate in the global healthcare fraud detection market are International Business Machines Corporation (IBM), Optum, Verscend Technologies, McKesson Corporation, FAIR ISAAC Corporation, SAS Institute Inc., HCL Technologies, Wipro Limited, Conduent, CGI Group, DXC Technology Company, UnitedHealth Group, Exlservice Holdings Inc., Scio inspire Corp, LexisNexis, OSP Labs, Northrop Grumman.
The forecast period for healthcare fraud detection market is 2022 to 2031.
The base year is 2021 for healthcare fraud detection market.
Loading Table Of Content...
Loading Research Methodology...



